JAMDA:对OS想要了解更多?来看看吧
2015-04-01 QQduhq 译 MedSci原创
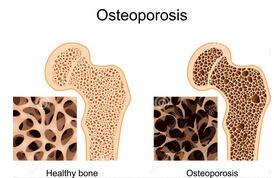
目的:在老年人群中,骨质减少/骨质疏松症与肌肉减少症已经成为身体虚弱人群发生入院、意外跌倒和损伤的高风险因素。然而, OS病人的特异性临床表现、生化指标和机体功能状态我们至今都不清楚。在这项研究中,我们使用osteosarcopenia作为OS临床命名,目的是为确定曾经跌倒过的老人特有的的临床表现、功能状态、生化特征等。设计:该研究为横断面研究。环境:试验在澳大利亚彭里斯尼平医院的一个骨外科门诊进
设计:
环境:
试验在澳大利亚彭里斯尼平医院的一个骨外科门诊进行。
参与人员:
我们对2009年至2013年于门诊就诊的共有680名、平均年龄为79岁的患者进行了实验调查,其中女性占65%。
干预措施:
我们对患者的评估包括病史询问、体格检查、骨密度测量、使用双能X线骨密度仪和姿势描记法检测记录身体骨骼构成、测试握力、步态参数,并且进行了与营养不良和继发性骨质疏松症和肌肉减少症有关的血液测试。根据结果,我们把患者身体状况分为4组:(1)骨质疏松(BMD<–1.0SD);(2)肌肉减少症;(3)OS;(4)既非肌肉减少症也非骨质疏松症。我们采用单因素方差分析和χ2检验评估分析组间差异,并采用多变量线性回归评估组间机体功能状态与治疗措施之间的关联,且多变量逻辑回归分析评估OS组患者存在的风险因素。
结果:
结论:
通过实验我们已经得知与OS患者密切相关的一系列临床特征,这项研究可以用于未来的实验设计提供方案设计指导,而且可以为患OS这个疾病的高风险人群提供干预措施以避免不良预后和机械治疗措施。
原始出处:
Huo YR, Suriyaarachchi P, Gomez F, Curcio CL, Boersma D, Muir SW, Montero-Odasso M, Gunawardene P, Demontiero O, Duque G.Phenotype of osteosarcopenia in older individuals with a history of falling.J Am Med Dir Assoc. 2015 Apr 1;16(4):290-5. doi: 10.1016/j.jamda.2014.10.018. Epub 2014 Dec 12.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了,好网站好文章
121
#MDA#
35
有指导意义
145
患OS这个疾病的高风险人群提供干预措施以避免不良预后和机械治疗措施
134
确实有指导意义,谢谢
103
确实有指导意义
64
什么是横断面研究?
124
有意义
81
对健康指导有意义
84
#AMD#
35