春季易发的9种过敏性皮肤病
2022-03-29 药店网校 药店网校
春天来了,春暖花开,阳光明媚。但是有些皮肤病也随之而来,折磨着很多人。我们一起来看下春季有哪些易发的皮肤病呢?
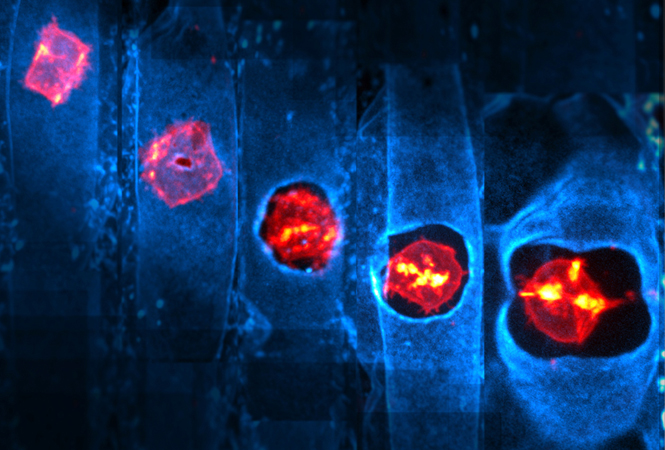
1 湿疹 湿疹是一种常见病,是由多种内、外因素引起的皮肤炎症,其病因复杂,一般认为与变态反应有关。 2 药疹 药疹又称药物性皮炎,是药物通过口服、注射、吸入、栓剂吸收、外用透皮吸收等途径进入人体后引起的皮肤黏膜反应。 可以引起药疹的药物很多,最常见的有抗生素类药、磺胺类药、镇静药和解热镇痛药、异种血清制剂及疫苗等。 1.症状: 1)固定红斑型:这是最常见的一型。好发于手足背及皮肤黏膜交界处,如口唇、外生殖器、肛门等处。 皮疹特点是圆形或椭圆形的水肿性紫红斑,直径一般1~2cm或更大,境界清楚,多数是单发,少数也可多发,紫红斑中央可出现水疱或大疱,持续7~10天,消退后留有暗褐色或棕褐色色素沉着斑,可持续数月或更长时间。自觉症状仅有轻度痒感及灼痛感。 如再次用致敏药物,又会在原处发生同样皮疹,随着复发次数增加,皮损数目亦可增多,面积可扩大。反复发作后,遗留的色素沉着斑不易消退。 2)荨麻疹性药疹:较常见。症状与急性荨麻疹相似,但风团颜色较鲜红,皮疹持续时间较长。严重的可伴有发热、关节痛、淋巴结肿大、血管性水肿和蛋白尿等。 3)麻疹样或猩红热样型:皮肤上出现弥漫性鲜红色斑或半米粒大的红色斑丘疹,皮疹主要分布于躯干,可泛发全身,类似麻疹或猩红热。 4)多形红斑型:特点是豌豆大至蚕豆大圆形或椭圆形水肿性红斑或丘疹,中央常有水疱,对称发生于四肢伸侧、躯干,境界清楚,有痛痒感。重症病人的口、眼、外阴黏膜会发生水疱糜烂,剧烈疼痛。 5)大疱性表皮松解型,这是药疹中最严重的一型 可发生于任何年龄,起病急骤,全身中毒症状明显,皮肤出现弥漫性紫红或暗红斑片,并很快出现松弛性水疱、大疱及表皮大片松解脱落,疱壁易被撕破和脱落,露出糜烂面,渗液较多。 同时有高热、疲乏、咽痛、呕吐、腹泻等症状,容易继发感染,发生肝肾功能障碍,电解质紊乱或内脏出血。此病死亡率高,应当送患者及时就医。 2.特点:任何一种药物,包括保健品在内都可能引起药疹。 3.病因:可以引起药疹的药物很多,最常见的有抗生素类药、磺胺类药、镇静药和解热镇痛药、异种血清制剂及疫苗等。 4.鉴别: 1)麻疹样或猩红热样型药疹与麻疹或猩红热 区别是麻疹或猩红热没有近期用药史,并且出现皮疹前有上呼吸道症状(感冒,流涕,咳嗽,头痛等);而麻疹样或猩红热样型药疹没有上呼吸道症状,且有近期用药史。 如果在发病前20天内使用了以前未用过的药物,或以前用过但此时服用时药物已过期,或此次服用的和以前的非同一药厂生产,就可诊断为药疹; 2)多形红斑型药疹与多形红斑:区别在于后者无近期用药史。 5.治疗: 局部治疗可使用:炉甘石洗剂、氧化锌软膏、外用糖皮质激素制剂、外用抗菌药制剂等。 口服药物可选择:抗组胺药、口服激素、雷公藤多甙片。 3 荨麻疹 荨麻疹,俗称“风疹块”,是由于皮肤、黏膜小血管反应性扩张及渗透性增加而出现的一种局限性水肿反应,产生红斑和风团,伴瘙痒。 荨麻疹的病因复杂,约3/4的患者找不到原因。其常见类型有急性和慢性两种。 1.症状: 1)急性荨麻疹:皮疹为大小不等的红色或苍白色风团,风团大小和形态不一,发作时间不定,数小时内风团可出现或消失。 部分患者可伴有恶心、呕吐等症状,甚至出现喉头水肿、呼吸困难或窒息。 2)慢性荨麻疹:全身症状一般较轻,风团时多时少,反复发生,病程在6周以上。 2.特点:花粉诱发的荨麻疹,春季多发。 3.病因:病因复杂,约3/4的患者找不到原因。但空气中的花粉、尘螨等是重要的诱因。 4.鉴别:注意与荨麻疹性血管炎、丘疹性荨麻疹鉴别。 5.治疗:去除可能的诱因,长期反复者,最好查过敏原,针对性避免或脱敏治疗;口服抗组胺药;严重者必要时使用激素或免疫抑制剂。 4 季节性面部皮炎 为一种好发于春季,由花粉等引起的皮炎。多见于女性。 1.症状:颜面、颈部轻度红斑、丘疹、肿胀,伴瘙痒,严重的可出现渗液,后期可皮肤轻度肥厚,有脱屑。 2.特点:春季好发,每年反复发生,轻者过了春季可自行消退。有些人伴有过敏性鼻炎或哮喘等。 3.病因:空气中的花粉。可查过敏原明确。 4.鉴别:需要与化妆品皮炎及日光性皮炎鉴别。 5.治疗:应注意皮肤的清洁、保湿;对症抗过敏治疗;如长期反复发生,比较严重的,最好查过敏原,针对性脱敏治疗。 5 日光性皮炎 是一种常见的对日光中紫外线过敏的疾病,好发于春季和夏初。 1.症状:在曝光部位出现境界清楚的红斑,鲜红色;随后红斑颜色变暗、脱屑,留有色素沉着或减退。自觉烧灼感或刺痛感,常影响睡眠。 2.特点:主要分布于面、颈及手背等暴露部位,一般在日晒后数小时或数天出现。 3.病因:日光中的紫外线。可做光敏试验明确。 4.鉴别:注意与接触性皮炎和红斑狼疮鉴别。 5.治疗:防晒;对症抗炎治疗;可口服硫酸羟氯喹抗光敏;尽量避免吃光敏性食物或药物,如香椿、香菜、芹菜、黄泥螺、皮皮虾、磺胺、四环素类药物等。 6 激素依赖性皮炎 由长期不恰当使用外用软膏的激素引起,因为症状类似吸毒成瘾,停用后皮炎反复加重,又称为激素成瘾性皮炎、激素戒断皮炎。 1.症状:皮肤出现明显鲜红色斑,表面光滑、变薄、毛细血管扩张、干燥、脱屑等。遇热症状加重。 2.特点:最常见于面部,多数有刺痛、烧灼和瘙痒感。 3.病因:长期反复外用激素≥1月。 特别小心:有些不正规的面膜或护肤品中含有激素,这些产品的特点就是短期内效果奇好。 4.鉴别:需要和口周皮炎、激素过敏及原发皮肤病停药复发鉴别。 5.治疗: 停用一切外用激素; 保湿:增加角质层内水分,恢复皮肤屏障; 抗炎:局部外用免疫调节剂,如他克莫司软膏、吡美莫司软膏,口服抗组胺药,如氯雷他定片或依巴斯汀片等。 如继发感染,需要同时使用抗生素。 7化妆品皮炎 是指由化妆品刺激或过敏引起的皮肤病。 1.症状:出现红斑、丘疹,严重者出现水疱、渗液,自觉瘙痒。 2.特点:常见于面部使用化妆品的部位,停用后缓解,再次使用复发。 3.病因:对化妆品中的一些成分过敏,如肉桂醛、苯甲醇、熏衣草油、依兰油、颜料、香精等。必要时可以做斑贴试验明确过敏原。 4.鉴别:根据明确的化妆品接触史可与其他过敏性皮炎区别。 5.治疗:停用并及时清除皮肤残留的引起过敏的化妆品;抗过敏治疗;可使用适合敏感皮肤的医学护肤品。 8 丘疹性荨麻疹(虫咬性皮炎) 是由昆虫叮咬皮肤引起的过敏性皮肤病,又称虫咬性皮炎、单纯性痒疹,春秋多见。 常分批发生于躯干、四肢伸侧,自觉瘙痒。皮损为红色风团样丘疹,呈纺锤形或圆形,中央常有丘疱疹、水疱或大疱。 1.症状:局部红肿,常呈梭形,表面可出现水疱及大疱,皮损中心有时可见叮咬痕迹。自觉奇痒,有时有刺痛、灼疼。 2.特点:尽管成人也可发生,但最常见于儿童,而且比较重。 3.病因:常由蚊、白蛉、蠓、蚋、臭虫、蚤、虱、螨虫及其他昆虫叮咬引起。 4.鉴别:注意和荨麻疹鉴别:后者多发于夏秋季节,儿童尤多,为风团样丘疹性皮疹,可与某些昆虫如蚊虫、螨、跳蚤、臭虫等叮咬有关,且风团样丘疹不会时起时消。 5.治疗: 注意个人及环境卫生,对于易发生本病的患者,在春秋季节尽量少到花草多的地方; 一般可外用炉甘石洗剂、激素软膏,合并感染时可给予抗菌素。 有全身症状可用抗组胺药物,如果非常严重,必要时使用激素治疗。 9 接触性皮炎 接触性皮炎是皮肤或黏膜接触某种物质后,在接触部位发生的急性或慢性炎症反应。 1.症状:主要表现为红斑,肿胀,丘疹,水疱,甚至大疱。急性接触性皮炎皮疹只局限于接触部位,并且皮疹形状与接触物形状一致。如果接触物为长方形,其边界很清楚。 2.特点:只局限于接触部位,并且皮疹形状与接触物形状一致。去除接触物,适当处理后皮损一般很快消退。 3.病因:能引发接触性皮炎的物质有很多种,可分为动物性、植物性和化学性三大类。在医院,斑贴试验是诊断接触性皮炎的最简单可靠的方法。 1)动物性物质包括动物毒素,如昆虫分泌物、毒毛等; 2)植物性物质包括花粉、叶、茎、花及果实等; 3)化学性物质是引起接触性皮炎的主要原因,主要有金属及其制品、塑料、橡胶、香料等。 4.鉴别: 1)接触性皮炎与急性湿疹:急性湿疹的病因一般不明确,发病常呈泛发性,损害呈多形性,病程较长,且有复发倾向。急性接触性皮炎的接触史明显,病变局限于接触部位,皮疹形状与接触物形状一致,搔抓后可将致病物质带到远隔部位并产生类似皮损。 2)面部接触性皮炎与皮肌炎:后者多发生于双上睑,为水肿性紫红,伴有全身无力症状和肌酶谱升高等。 5.治疗: 口服药:抗组织胺药类:皿治林、氯雷他定、西替利嗪、荨麻疹丸。 外用药:丹皮酚、曲咪新软膏、艾洛松、皮炎平。 联合用药:维生素C或B族、钙剂、氨基酸软胶囊、氧氟沙星凝胶。 常见治疗方法 ①轻度皮肤过敏 如果只有轻微的红斑、少量细小鳞屑,无明显水肿,瘙痒不明显者,只需尽量避免诱发因素,同时使用医学护肤品的保湿舒敏系列产品,可以不用药物。 ②中度皮肤过敏: 有红斑、丘疹、水肿,伴明显瘙痒者,可短期使用激素软膏,如丁酸氢化可的松软膏、地奈德软膏或糠酸莫米松乳膏,但连续使用最好不超过2周,而且应在病情好转后逐渐减量停药。 如果长期反复发生,则最好外用免疫调节剂,如0.03%他克莫司软膏或吡美莫司软膏。可口服抗组胺药,如氯雷他啶片或依巴斯汀片等,也可配合使用复方甘草酸苷片。 ③重度皮肤过敏: 除了中度过敏的症状,还出现水疱和流黄水。则需要用2%硼酸溶液或生理盐水冷敷,将4~6层纱布浸湿拧干,以不滴水为度,敷于面部红斑处。 湿敷时保持纱布冷湿,每次15~20分钟,每天2~3天。冷敷后短期使用激素类软膏或免疫调节剂软膏(同前)。 如果一般抗过敏药效果不佳,需要短期全身使用激素,一定要注意药物的不良反应。如继发感染,则需要口服或外用抗生素。 ④荨麻疹:应以口服抗组胺药为主,一般没有必要外用药。 ⑤丘疹性荨麻疹(虫咬性皮炎):应以外用药为主,严重的可配合口服药。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#皮肤病#
63
#过敏性#
53
学习了#过敏#
65
学习并收藏了
54
受益匪浅
49
学习#学习#
51
学习#期刊论坛#
95
好好学习
57