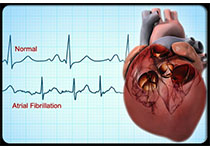
病例解读:心律失常的社区处理
2017-10-26 张剑(天津市滨海新区杭州道街向阳社区卫生服务中心全科主治医师) 医师在线
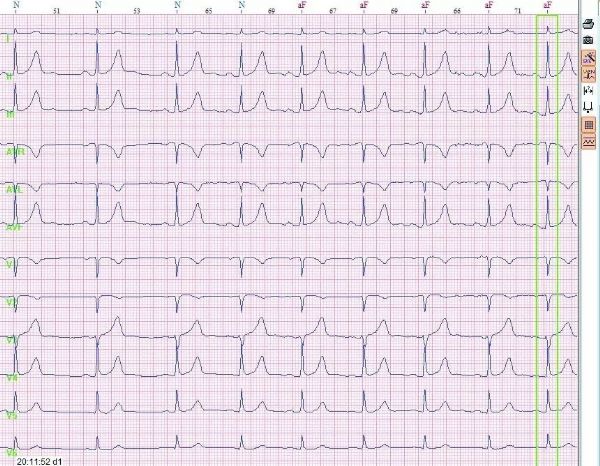
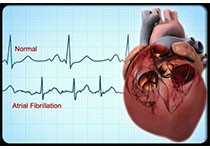
面对这样一份复杂的心律失常心电图,我觉得没有能力阅读,社区医院也没有能力处理这样复杂的心律失常。于是将该患者转到上级医院,接诊大夫建议该患者做射频消融手术。当时大夫给出的具体诊断不详。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了谢谢作者分享!
52
学习
0
#社区#
32
学习了新知识
67
谢谢了.学习
67
学习了新知识学习了新知识
49
谢谢分享.学习了
28
好
28
学习
28
阅读.谢谢分享.
28