EUR J Cancer:伊匹单抗单独使用或与nivolumab联合使用治疗晚期黑色素瘤
2017-12-30 MedSci MedSci原创
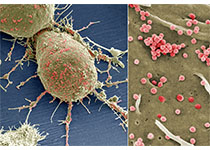
Ipilimumab作为一种单克隆抗体,能有效阻滞一种叫做细胞毒性T细胞抗原-4(CTLA-4)。CTLA-4会影响人体的免疫系统,削弱其杀死癌细胞的能力。
Ipilimumab作为一种单克隆抗体,能有效阻滞一种叫做细胞毒性T细胞抗原-4(CTLA-4)。CTLA-4会影响人体的免疫系统,削弱其杀死癌细胞的能力。
相比于ipilimumab单药治疗,程序性细胞死亡蛋白-1(PD-1)抑制剂派姆单抗(pembrolizumab)和nivolumab单独或与ipilimumab联合使用,能够显著改善晚期黑色素瘤患者的客观反应率和无进展生存期。然而ipilimumab单独或与nivolumab联合治疗PD-1抗体耐受的晚期黑色素瘤的证据依然较少,为此研究者们进行了一项多中心回顾性分析,临床试验中的药物剂量如下所示:nivolumab(1mg或3mg / kg)和ipilimumab(1mg或3mg / kg)或ipilimumab(3mg / kg)。
对于PD-1抗体治疗后无效的患者,共有47例患者接受了ipilimumab(ipi-group)治疗和37例患者的接受了ipilimumab / nivolumab联合治疗。单药组和联合组的总体应答率分别为16%和21%;单药的疾病控制率为42%,联合组为33%。单药组和联合组的总生存率分别为54%和55%。
因此,就总体应答率而言,Ipilimumab应被视为PD-1抗体治疗失败后的可行方案。
原始出处:
Zimmer, Lisa, et
al. "Ipilimumab alone or in combination with nivolumab after progression
on anti-PD-1 therapy in advanced melanoma." European Journal of Cancer 2017
75: 47-55. doi.org/10.1016/j.ejca.
本文系梅斯医学(MedSci)原创编译整理,转载需授权
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#mAb#
44
#色素#
21
#NIV#
30
#黑色素#
38
#黑色素#
31