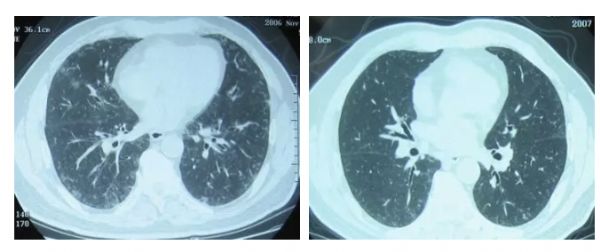
症状很像慢阻肺,许多患者戒了烟就能康复……呼吸性细支气管炎伴间质性肺疾病鉴别诊断难在哪?
2018-12-09 代华平、谢冰冰 呼吸界
大部分医务工作者乃至患者都清楚吸烟是引发肺癌的元凶,但吸烟对呼吸系统的伤害远不止此,本文共提到4种纤维化性肺疾病,其中大部分甚至所有都与吸烟有密切关系!对于「吸烟相关性间质性肺疾病」的检查结果有何特征、怎样鉴别诊断、首选哪些治疗,不少临床医生还不够了解,为此,中日友好医院呼吸与危重症医学科代华平主任进行了权威解读。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#细支气管#
45
#细支气管炎#
49
#间质性#
42
#支气管#
43
#间质性肺疾病#
51
#鉴别诊断#
41