NAT BIOMED ENG:朝阳医院陶勇团队等提出外泌体联合VEGF,治疗眼底新生血管性疾病
2021-08-01 “E药世界”公众号 “E药世界”公众号
2021年7月26日,首都医科大学附属北京朝阳医院陶勇教授联合中科院过程工程所生化工程国家重点实验室魏炜研究员团队和澳大利亚昆士兰大学T细胞免疫机制及监控实验室余迪教授团队开展学科交叉合作,在 Nat
眼底新生血管的形成是年龄相关性黄斑变性、糖尿病视网膜病变等多种眼底疾病发生过程中的重要环节,若得不到有效治疗将严重影响视功能,甚至导致视力的丧失,给患者的生活和工作带来极大不便。
目前,玻璃体腔注射血管内皮生长因子(VEGF)抗体是临床治疗眼底新生血管性疾病的主要策略,但仍然存在药物随房水代谢过快、难以富集眼底病灶和单一治疗策略效果有限的难题。因此,即便多次注射,临床实际响应率也仅为40%~60%。
2021年7月26日,首都医科大学附属北京朝阳医院陶勇教授联合中科院过程工程所生化工程国家重点实验室魏炜研究员团队和澳大利亚昆士兰大学T细胞免疫机制及监控实验室余迪教授团队开展学科交叉合作,在 Nature 子刊 Nature Biomedical Engineering 发表了题为:Reduction of choroidal neovascularization via cleavable VEGF antibodies conjugated to exosomes derived from regulatory T cells 的研究论文。提出了优于现有的单独VEGF抗体治疗的新策略。
陶勇教授多年从事眼底新生血管性疾病临床诊疗工作,通过建立眼内液临床样本库和发展微流控眼内液检测方法,发现眼底新生血管性疾病不仅含有高水平的VEGF,而且富集了IL-6、IL-1β、TNF等大量的炎症因子,并且相互之间具有明显的正相关性,揭示了眼底新生血管发生发展过程中血管新生和炎症之间的紧密互作关系,并以此提出了“抗VEGF-抗炎”协同治疗的新思路。
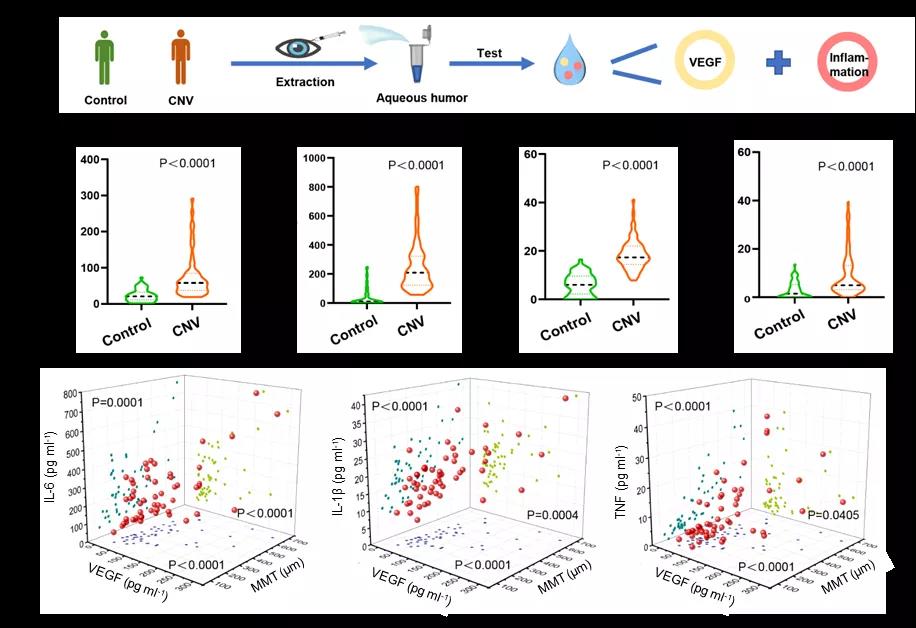
图1:房水检测揭示眼底新生血管形成过程中血管新生和炎症之间的紧密互作关系:a.临床房水样本采集及VEGF和炎症因子检测示意图;b.检测CNV患者房水中VEGF和炎症因子(IL-6、IL-1β、TNF)的含量;c.VEGF、炎症因子(IL-6、IL-1β、TNF)与CNV病情严重程度的相关性分析。
在此基础上,陶勇教授团队与魏炜研究员团队和余迪教授团队联手合作,利用体内具有天然抗炎活性的基于调节性T细胞外泌体(rEXS)为载体,通过基质金属蛋白酶(MMP)敏感肽段(cL)连接VEGF抗体(aV),创建了rEXS-cL-aV体系。当玻璃体腔注射后,利用rEXS向炎症部位的趋化性,携带aV富集于眼底新生血管病灶,随后利用病灶部位高表达的MMP酶解敏感肽段cL并释放aV。在上述时空耦合递送的基础上,分别利用rEXS的抑制炎症作用和aV的抑制血管生成作用实现协同增效。在小鼠和食蟹猴的脉络膜新生血管模型中,单次注射即可显着抑制新生血管性疾病的发生和发展,并且效果显着优于现有的单独VEGF抗体治疗策略。
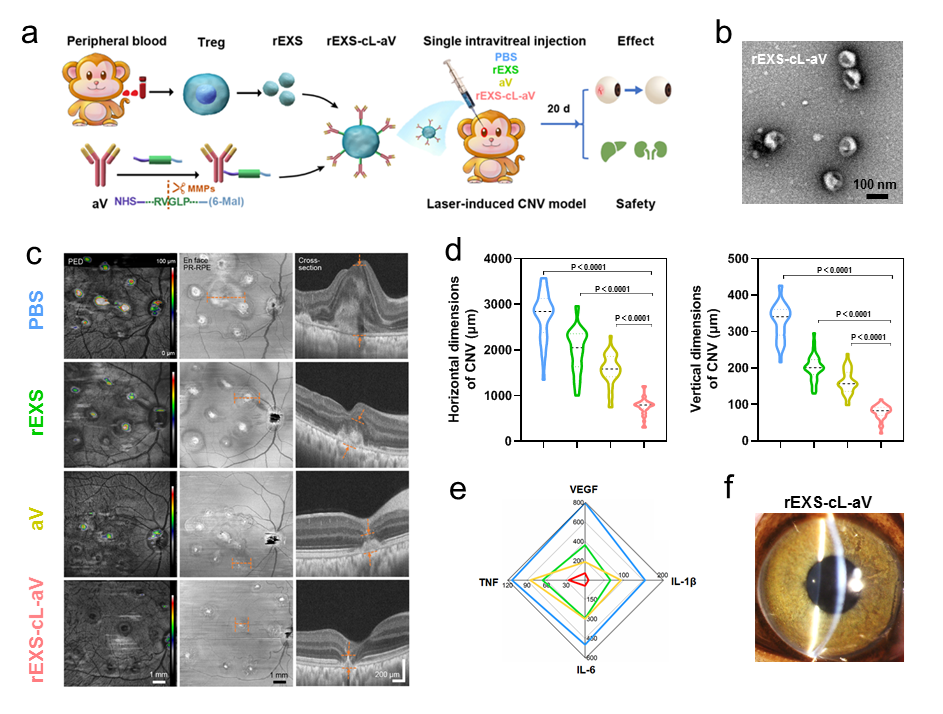
图2:rEXS-cL-aV在食蟹猴CNV模型的抗新生血管疗效和安全性验证:a. rEXS-cL-aV的构建及在食蟹猴CNV模型中治疗策略示意图;b. rEXS-cL-aV透射电子显微镜成像图;c. 光学相干断层扫描血管成像分析rEXS-cL-aV在食蟹猴CNV模型中治疗效果;d. 定量分析图c中病灶范围;e. 食蟹猴各组给药后房水中VEGF,IL-6,IL-1β及TNF含量检测;f. 玻璃体腔注射rEXS-cL-aV后裂隙灯观察眼前节情况。图片来源:Nature Biomedical Engineering
“眼底新生血管性疾病是重要致盲原因,传统的单一抗VEGF治疗仍有局限性,开发新的治疗手段具有重要的临床意义。通过巧妙的方法连接外泌体与VEGF抗体,达到抗炎抗VEGF双重效果,实现治疗的空间和时间耦合,这是一项很有实用前景的创新性研究。”中国工程院院士谢立信如是评价道。
据研究人员介绍,上述成果仍属于动物水平的临床前研究,实际临床疗效仍有待进一步研究。鉴于自体细胞组分和已批准抗体的安全性、治疗结果的有效性和重现性,该制剂具有较好临床转化潜力。研究团队正在按照相关要求合作推进临床个体化治疗的研究。
“未来,我们将继续将外泌体与不同细胞因子抗体进行连接,实现多重调控,拓宽治疗效果,并在干眼症、黄斑水肿等其他眼病探索新型治疗研究,完善临床实验前的研究工作,争取早日让眼病患者享受到这一技术。”陶勇在接受《中国科学报》采访时表示。
据了解,陶勇教授团队在眼底新生血管性疾病新机制新靶点研究领域;眼内液检测领域,眼底疾病精准诊断与疗效监测领域和眼底疾病药物递送系统的研发等领域积累了雄厚的工作基础和业绩。相关工作相继发表于 Archives of Ophthalmology、Journal of Materials Chemistry、Retina、IOVS、J Mater Chem B、Chemical Communications、Acta Biomaterialia 等眼科和生物医药领域国际知名学术期刊上。
此项工作是该团队基于以往的研究基础,在眼底病治疗领域的新突破。田颖博士和张帆博士为共同第一作者,陶勇教授、魏炜研究员、余迪教授为共同通讯作者。相关工作得到了国家自然科学基金面上项目、北京市教委科技计划项目和北京朝阳医院人才培养计划的支持。
原始出处:
Cohen, C.A., Li, A.P.Y., Hachim, A. et al. SARS-CoV-2 specific T cell responses are lower in children and increase with age and time after infection. Nat Commun 12, 4678 (2021). https://doi.org/10.1038/s41467-021-24938-4.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











了解到了新知识,有用处!
34
棒
48
#新生血管#
47
#Bio#
44
#Nat#
37
#血管性#
0
学习
52
#Eng#
42
#陶勇#
32
#VEGF#
53