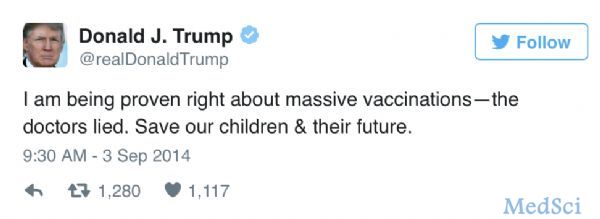
NAT MED:“神药”二甲双胍又有新用!改善自闭症社交能力
2017-05-17 佚名 生物探索
脆性X综合征是一种常见的遗传性智力低下疾病,由X染色体上一个名为FMR1的基因的遗传缺陷引起。近日,发表于Nature Medicine上的一项研究发现,糖尿病药物二甲双胍可改善社交能力,减少成年小鼠脆性X综合征的症状行为。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
22
#自闭#
31
#社交#
41
#Med#
25
真棒
62