Int J Pediatr Otorhinolaryngol:脑膜炎后耳聋患者植入人工耳蜗的听觉和语言改善如何?
2022-04-01 AlexYang MedSci原创
尽管因脑膜炎而失聪的受试者从人工耳蜗植入中获益匪浅,但我们发现这些患者的脑膜炎病史与异常的CAP和SIR结果之间存在中度至强的关系。
近日,来自伊朗设拉子医科大学的研究人员研究鉴定了细菌性脑膜炎后深度感音神经性耳聋(SNHL)患者的听觉、语言和手术效果。相关研究结果发表在《International Journal of Pediatric Otorhinolaryngology》期刊上。
2003年至2020年期间接受单侧人工耳蜗植入的双侧重度至极重度SNHL患者被纳入这项历史队列研究。研究的主要结果通过听觉表现分级标准(CAP)和言语可懂度分级标准(SIR)的分数来评估。CAP和SIR结果是在术后三个时间点收集的,即6、12和24个月。为了获得关系的强度和用对数二项回归方法计算风险比(RR),研究人员在分析中对CAP和SIR使用了两种二元分类模型。
结果显示,研究组和对照组植入人工耳蜗时的平均年龄分别为144.30(156.90)和121.10(133.70)月。在研究组中,35名患者中有19名(54.3%)是男性,16名(45.7%)是女性。在对照组中,81名患者中有34名(42.0%)是男性,47名(58.0%)是女性。
在该研究中,两组患者的CAP和SIR的平均得分在这段时间内都有明显改善。所有的P值在两组中都是显著的(T2 vs T1,T3 vs T1,T3 vs T2)。研究人员通过对数二项回归分析,并根据CAP和SIR两种分类计算RR,显示这些患者是否有脑膜炎病史和异常的CAP和SIR结果之间存在中等至强的关系。
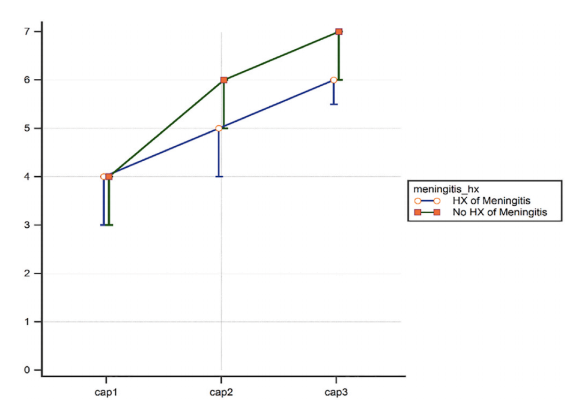
图1 T1 至 T3三个时间点的CAP评分中位数和IQR
综上所述,尽管因脑膜炎而失聪的受试者从人工耳蜗植入中获益匪浅,但我们发现这些患者的脑膜炎病史与异常的CAP和SIR结果之间存在中度至强的关系。
原始出处: Tayebeh Kazemi , Seyed Basir Hashemi , Najmeh Keshavarz et al. Auditory and speech outcomes of cochlear implantation in post-meningitis deafness. Int J Pediatr Otorhinolaryngol. 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
29
#DIA#
34
#人工耳蜗#
64
#语言#
38
#植入#
55