Clinical Infectious Disease: 静脉注射抗假单胞菌抗生素数量与小儿囊性纤维化肺加重临床结局的关系
2021-11-08 MedSci原创 MedSci原创
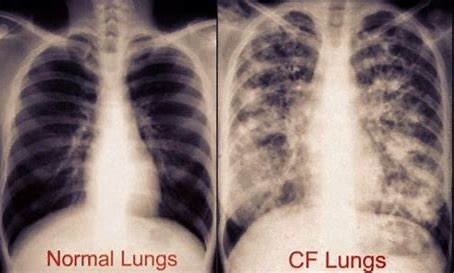
囊性纤维化是一种遗传性外分泌腺疾病,主要影响胃肠道和呼吸系统,通常具有慢性梗阻性肺部病变、胰腺外分泌功能不良和汗液电解质异常升高的特征。
囊性纤维化 (PwCF) 患者的肺部疾病加重 (PEx) 的发病率显著上升,这部分患者的生活质量会明显下降、肺功能和体重也会减轻。轻度至中度 PEx 通常使用口服抗生素和积极的气道清除来治疗,而严重的 PEx 通常需要静脉注射 (IV) 抗生素。在铜绿假单胞菌( Pa ) 感染患者中,通常同时使用2种IV抗假单胞菌抗生素进行治疗,理由是该策略可增强杀菌活性并减少耐药菌的选择。本研究旨在比较单一和双重抗假单胞菌抗生素用于 PEx 治疗的临床结果。

本项研究是一项回顾性队列研究,纳入的患者是2007年至2018年期间住院且年龄在 6-21 岁之间的PwCF患者。使用回归模型用于比较单静脉与双静脉抗假单胞菌抗生素方案之间的肺功能结果,最后使用倾向评分加权调整相关混杂因素进行更加精确的分析。
研究结果显示,在10660名PwCF患者中,总共收集到1080个PwCF患者中的2578 个 PEx数据,其中455名和 2123名PEx患者分别用1和2种IV抗假单胞菌抗生素治疗。在接受1和2种 IV 抗假单胞菌抗生素治疗的PEx 中, PEx 之间没有显着差异,入院时一秒用力呼气体积百分比 (ppFEV1)从基线下降的中位数分别为 13.8%(IQR,8.6-20.6)和 14.5%(IQR,9.1-21.7)。而PEx后3个月内恢复至基线 ppFEV1≥90% 的几率(优势比 0.83,[95% CI 0.61,1.13];P = 0.24)或下一次需要静脉注射抗生素的 PEx 时间(危险比) 1.04, [95% CI 0.87, 1.24]; P = 0.69)之间的差异也不明显。静脉注射抗生素治疗中加入吸入抗生素对PEx治疗没有临床益处。
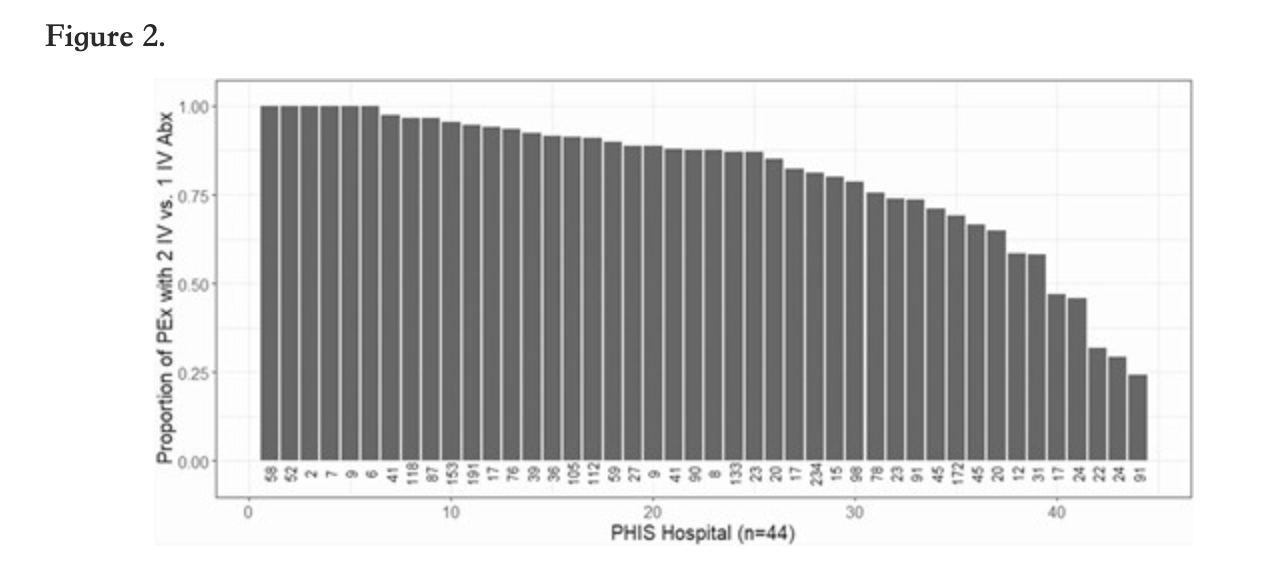
本项研究证实与使用1次IV抗假单胞菌抗生素治疗相比,在年轻PwCF患者中使用2种IV 抗假单胞菌抗生素进行PEx治疗与测量的呼吸和临床结果的更大改善无关。
原始出处:
Jonathan D Cogen. Et al. Association Between Number of Intravenous Antipseudomonal Antibiotics and Clinical Outcomes of Pediatric Cystic Fibrosis Pulmonary Exacerbations. Clinical Infectious Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#囊性#
64
#临床结局#
47
#Dis#
49
#静脉#
47
#静脉注射#
83
#clinical#
39
学习了很好
102