NAT STRUCT MOL BIOL:酶的冻结作用使科学家提出新的癌症治疗观点!
2017-07-04 佚名 medicalxpress
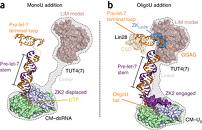
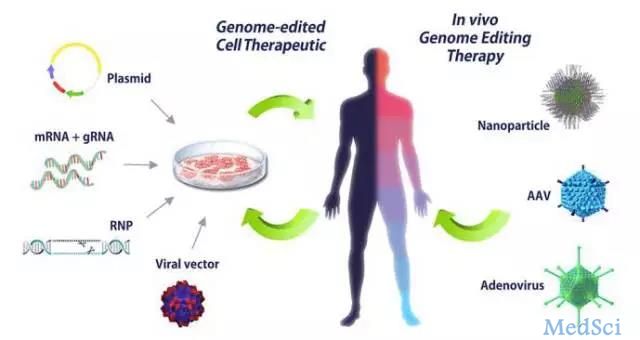
经过数百万年的发展,细胞已经开发出无数的方法来调节使它们蓬勃发展的过程。特别有用的工具已经被保存下来,或者是“保存”,所以今天我们可以从广泛的生命形式中找到它们,从原始到最复杂。 冷泉港实验室(CSHL)结构生物学家于2017年7月3日发表的研究揭示了一种这样的保守机制的运作,对新型癌症药物的发展具有重要意义。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Struc#
37
#Nat#
26
#Biol#
33
#Bio#
32
#癌症治疗#
31