Cancer Cell:揭示抑制肺癌恶化的新型疗法
2012-08-15 T.Shen 生物谷
肺癌是世界范围内最严重的癌症之一,尽管近些年来在肺癌分子生物学研究方面取得了很大进展,但是肿瘤细胞生长和扩散的机制目前并不清楚,因此开发相应的治疗方法也显得困难重重。 近日,来自西班牙国家癌症中心的研究者Manuel Serrano破解了肺癌背后的一种分子途径,通过此项研究,他们识别出的新的实验药物,在小鼠实验中可以阻碍癌症细胞的生长,相关研究成果刊登在了8月13日的国际著名杂志Cancer C

肺癌是世界范围内最严重的癌症之一,尽管近些年来在肺癌分子生物学研究方面取得了很大进展,但是肿瘤细胞生长和扩散的机制目前并不清楚,因此开发相应的治疗方法也显得困难重重。
近日,来自西班牙国家癌症中心的研究者Manuel Serrano破解了肺癌背后的一种分子途径,通过此项研究,他们识别出的新的实验药物,在小鼠实验中可以阻碍癌症细胞的生长,相关研究成果刊登在了8月13日的国际著名杂志Cancer Cell上。
勇敢地对抗肺癌
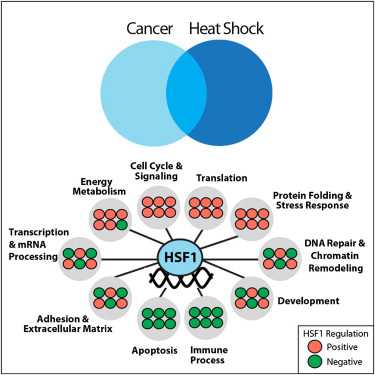
Notch途径是2004年发现的白血病发展的重要的癌基因,自从发现了该途径科学家投入了大量的精力来研究Notch途径在癌症中的作用。上世纪最后几年,研究者发现Notch途径也参与了胰腺癌和肺癌的发展。
这项研究中,研究者发现了Notch调节肺癌细胞增殖的分子途径,Notch途径蛋白可以和Ras癌基因协作,而Ras啊基因也是癌症发生的一个重要元件。于此同时,研究者也发现了一种特殊的实验药物的潜在治疗效应,他们使用遗传修饰的小鼠来进行实验,发现在15天的药物治疗后,小鼠的肺部肿瘤失去了生长发展的能力。
在人类和小鼠中进行联合临床试验
GSIs在治疗阿尔兹海默症上超过了15年历史,尽管目前已经知道GSIs不能有效阻止神经变性疾病,但是当前阻断Notch途径新药的发现也为该疾病的治疗提供了帮助。
小鼠的治疗试验和人类的同时开展,称为联合临床试验(coclinical trials)。这些试验在非常短的时间内允许信息在小鼠和人类之间进行转移,研究者认为,通过阻挡Notch途径对于治疗肺癌非常有帮助,Serrano博士说,我们已经用一种直接阻碍Notch途径蛋白功能的制剂来应用于病人,而且我们想扩大试验规模,我们预期结果会非常有希望的
编译自:New Therapy Prevents Lung Cancer Growth in Mice

doi:10.1016/j.ccr.2012.06.014
PMC:
PMID:
Therapeutic Effect of -Secretase Inhibition in KrasG12V-Driven Non-Small Cell Lung Carcinoma by Derepression of DUSP1 and Inhibition of ERK
Antonio Maraver, Pablo J. Fernandez-Marcos, Daniel Herranz, Marta Cañamero, Maribel Muñoz-Martin, Gonzalo Gómez-López, Francisca Mulero, Diego Megías, Marta Sanchez-Carbayo, Jie Shen, Montserrat Sanchez-Cespedes, Teresa Palomero, Adolfo Ferrando, Manuel Serrano
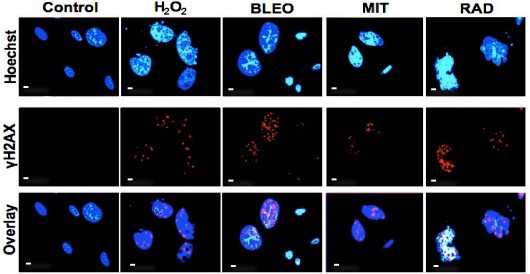
Here, we have investigated the role of the Notch pathway in the generation and maintenance of KrasG12V-driven non-small cell lung carcinomas (NSCLCs). We demonstrate by genetic means that -secretase and RBPJ are essential for the formation of NSCLCs. Of importance, pharmacologic treatment of mice carrying autochthonous NSCLCs with a -secretase inhibitor (GSI) blocks cancer growth. Treated carcinomas present reduced HES1 levels and reduced phosphorylated ERK without changes in phosphorylated MEK. Mechanistically, we show that HES1 directly binds to and represses the promoter of DUSP1, encoding a dual phosphatase that is active against phospho-ERK. Accordingly, GSI treatment upregulates DUSP1 and decreases phospho-ERK. These data provide proof of the in vivo therapeutic potential of GSIs in primary NSCLCs.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
32
#Cell#
28
#cancer cell#
23
#新型疗法#
32