Br J Clin Pharmacol:哪些因素会影响患者使用降压药的依从性?
2017-05-31 贾朝娟 环球医学
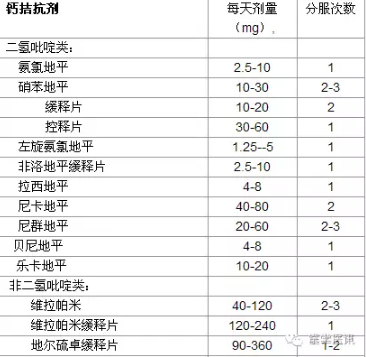
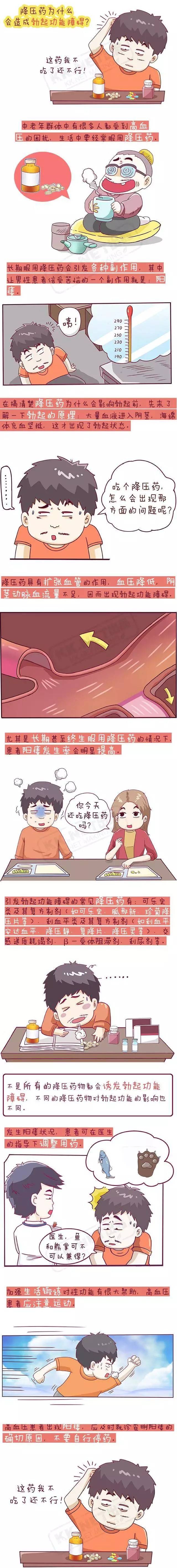
使用降压药的依从性差会影响治疗效果。2017年4月,发表在《Br J Clin Pharmacol》的一项研究显示,经历ADEs和对治疗不满意与较低的依从性相关。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Pharmacol#
20
#Pharm#
19
#pharma#
35
#MAC#
31
#降压#
30
#依从性#
24
学习了分享了
51
学习
42