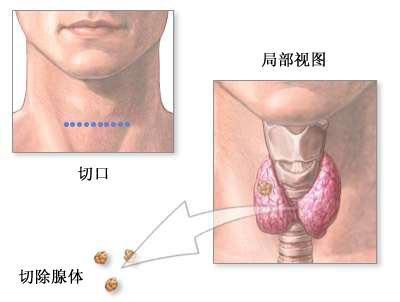
AIM:甲状旁腺切除术可降低患者未来骨折的风险
2016-04-05 崔倩 译 MedSci原创
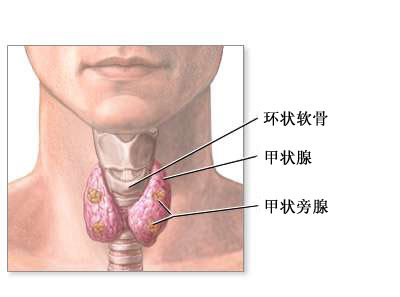
对于原发性甲状旁腺功能亢进症(PHPT),手术和药物治疗对于骨折的风险差别是未知的。该研究的目的是评估在PHPT患者中,甲状旁腺切除和双膦酸盐治疗对于这些患者骨骼的结果。该回顾性队列研究在一家集成医疗服务体系中进行,所有的参与者均为在1995到2010年期间确诊为PHPT的患者。检测主要指标为骨密度变化与骨折发生率。在2013例经过一些列骨密度检查的患者中,全髋BMD在甲状旁腺切除(在<2年
手术或药物治疗原发性甲状旁腺功能亢进症(PHPT),造成的骨折的风险差别是未知的。该研究的目的是评估在PHPT患者中,甲状旁腺切除和双膦酸盐治疗对于这些患者骨骼的结果。
该回顾性队列研究在一家集成医疗服务体系中进行,所有的参与者均为在1995到2010年期间确诊为PHPT的患者。检测主要指标为骨密度变化与骨折发生率。
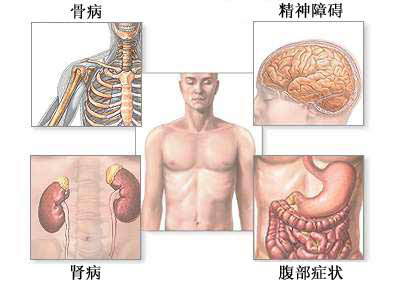
在2013例经过一系列骨密度检查的患者中,全髋BMD在甲状旁腺切除(在<2年时4.2%)和双膦酸盐(在<2年时3.6%)治疗的女性中短暂的增加,而在那些没有用这些治疗方法的女性和男性中逐渐下降(在>8年时,分别为-6.6%和-7.6%)。在随访时发生骨折的6272例患者中,在10年时髋部骨折的绝对风险为:每1000例患者发生——(甲状旁腺切除)20.4例事件 vs (双膦酸盐治疗)85.5例事件 vs (没有用这些治疗方法)55.9例事件。在10年时任何骨折风险对于甲状旁腺切除、双膦酸盐治疗以及不用这些方法治疗的患者中,事件发生率分别为每1000例患者发生156.8例事件 vs 302.5例事件 vs 206.1例事件。
在基线BMD状态分层的分析中,甲状旁腺切除术减少了骨质疏松和骨质疏松症患者骨折的风险,而双膦酸盐却增加了这些患者骨折的风险。不管患者是否满足手术相关指南,甲状旁腺切除术都减少了患者骨折的风险。该研究的限制性为回顾性研究设计和非随机治疗分配。
甲状旁腺切除术可降低骨折的风险,但双膦酸酯治疗并不优于手术治疗。
原始出处:
Michael W. Yeh,Hui Zhou,Annette L. Adams,et al.The Relationship of Parathyroidectomy and Bisphosphonates With Fracture Risk in Primary Hyperparathyroidism,Ann Intern Med,2016.4.5
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









好文,值得学习,赞!
75
#切除术#
35
#甲状旁腺#
38
#甲状旁腺切除术#
41
学习了,很好
118