ATS:纵隔淋巴结阴性的NSCLC可从同期寡转移灶切除中获益
2014-05-19 佚名 dxy
目前,肺癌已成为恶性肿瘤的头号杀手。据报道约30%-50%非小细胞肺癌(NSCLC)患者术后发生转移,且大部分转移或复发患者通过单种治疗方法病情无法控制。 然而,迄今为止,NSCLC局部转移患者外科手术切除的疗效仍然存在争议。研究证实,部分经严格筛选的NSCLC患者可从同期切除单个转移灶中获益。鉴于IV期NSCLC患者未行手术治疗其中位生存期仅为3-4月。 为了明确患者的筛选标准、术后生存率以
目前,肺癌已成为恶性肿瘤的头号杀手。据报道约30%-50%非小细胞肺癌(NSCLC)患者术后发生转移,且大部分转移或复发患者通过单种治疗方法病情无法控制。
然而,迄今为止,NSCLC局部转移患者外科手术切除的疗效仍然存在争议。研究证实,部分经严格筛选的NSCLC患者可从同期切除单个转移灶中获益。鉴于IV期NSCLC患者未行手术治疗其中位生存期仅为3-4月。
为了明确患者的筛选标准、术后生存率以及预测根治性切除后的疗效因素等,来自德国柏林Heckeshorn肺科医院胸外科Pfannschmidt教授等就根治性治疗同期NSCLC寡转移患者的经验进行总结,文章于2014年5月发表在ATS杂志上。
该回顾性研究纳入了1997年至2009年间同期NSCLC寡转移(如单个肺部或肺外转移灶)行根治性切除的患者,共99例,中位年龄62岁。腺癌(n=68),鳞癌(n=22),大细胞癌(n=6)和其他(n=3)。肺内转移(n=57),脑转移(n=21),肾上腺转移(n=10),骨转移(n=4),肝和横膈转移(n=2),纵隔或胸腺转移(n=2),胸膜转移1例。
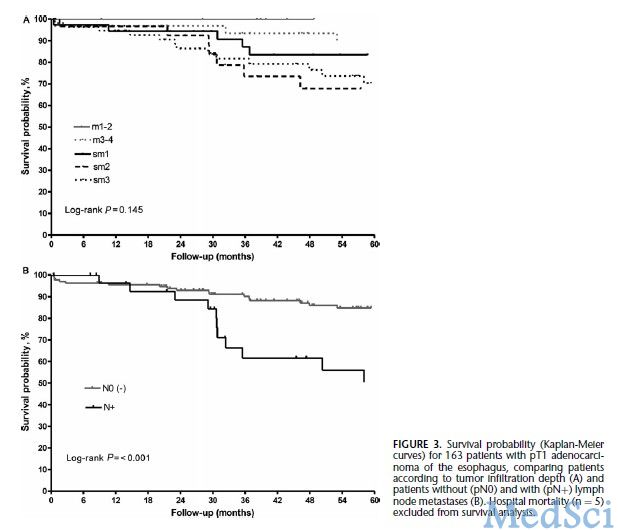
总的五年生存率为38%。无纵隔淋巴结转移(pN0/pN1)患者中位生存期为50个月,与pN2/pN3转移患者(中位生存期是19月)相比存在明显差异;pN0患者与pN1-N3患者相比其中位生存期亦有显著差异(如图1)肺内和肺外转移患者的中位生存期分别为56月、18月,五年生存率分别为48.5%、23.6%,其差异有统计学意义。
单变量生存分析显示,年龄、性别、组织学类型、病理T分期以及同侧/对侧肺内转移和围手术期化疗,对预后均无显著意义;COX回归分析表明,N分期较高和肺外转移是预后差的两个独立危险因素。
该研究显示,经严格筛选的部分患者反复转移灶切除亦可能使患者获益。然而,本研究存在很多局限,如回顾性研究的本质,病例数较少,研究时间区间较长等。尽管如此,由于NSCLC寡转移灶切除临床数据匮乏,该成果将成为未来进一步研究的焦点。
总之,无纵隔淋巴结转移NSCLC患者同期寡转移灶切除术安全有效,且N分期和肺转移的部位是远期生存率的两个独立危险因素。
原始出处
Tönnies M1, Pfannschmidt J2, Bauer TT3, Kollmeier J3, Tönnies S1, Kaiser D1.Metastasectomy for Synchronous Solitary Non-Small Cell Lung Cancer Metastases.Ann Thorac Surg. 2014 May 10
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ATS#
36
#转移灶#
40
#同期#
25
#淋巴结阴性#
26
#淋巴结#
30