NEJM:VEST研究发表:可穿戴式除颤器未发挥保护作用?穿戴时间不够或是原因之一
2018-09-28 朱柳媛 中国循环杂志
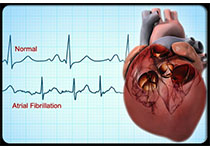
近年来,可穿戴式除颤器成为心律失常领域的一大研究热点。有心脏性猝死风险的人无需手术,只要穿戴上这种除颤器就可监测室性心律失常,一旦识别到恶性心律失常发生,除颤器就会报警并提醒即将放电,从而挽救患者的生命。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#EST#
35
#穿戴式#
39
#除颤#
36
#保护作用#
39