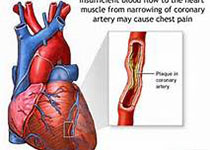
JAHA:冠脉搭桥术后6-12h的cTnT水平能预测患者预后
2018-02-28 MedSci MedSci原创
心肌肌钙蛋白T(cTnT)水平会在冠脉搭桥术后常规检测。本研究的目的旨在评估cTnT水平与冠脉搭桥术后6-12小时预后的关系。本研究纳入了1722名接受孤立性冠脉搭桥术的患者,评估了749名患者的传统cTnT水平和973名患者的高敏cTnT(hs-cTnT)水平与术后6-12小时主要心脑血管不良事件(MACCE)的发生的相关性。在传统cTnT评估组,有92名(12%)患者出现了MACCE,在hs-
心肌肌钙蛋白T(cTnT)水平会在冠脉搭桥术后常规检测。本研究的目的旨在评估cTnT水平与冠脉搭桥术后6-12小时预后的关系。本研究纳入了1722名接受孤立性冠脉搭桥术的患者,评估了749名患者的传统cTnT水平和973名患者的高敏cTnT(hs-cTnT)水平与术后6-12小时主要心脑血管不良事件(MACCE)的发生的相关性。在传统cTnT评估组,有92名(12%)患者出现了MACCE,在hs-cTnT评估组,有114名(12%)患者出现了MACCE。与cTnT ≤200 ng/L的患者相比,cTnT每增加200 ng/L,患者的MACCE的发生率更高,传统cTnT和hs-cTnT均能较好地区分出MACCE患者。以800 ng/L作为分界点,传统cTnT和hs-cTnT能为临床MACCE提供有效的支持力。研究结果显示,冠脉搭桥术后6-12h的心肌肌钙蛋白T水平可以提示患者的主要心脑血管不良事件发生的风险。原始出处:Brigitta G et al.Prognostic Value of Early Postoperative Troponin T in Patients Underg
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#cTnT#
31
#患者预后#
29
#冠脉搭桥术#
41
#搭桥#
21
#AHA#
38
#搭桥术#
23
#冠脉搭桥#
26
学习学习
65