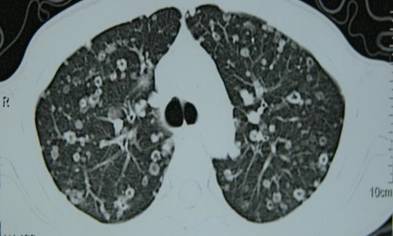
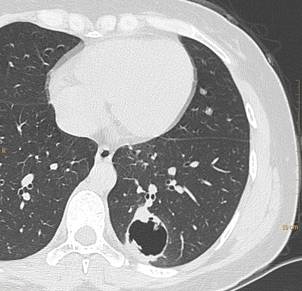
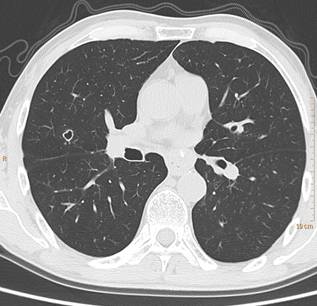
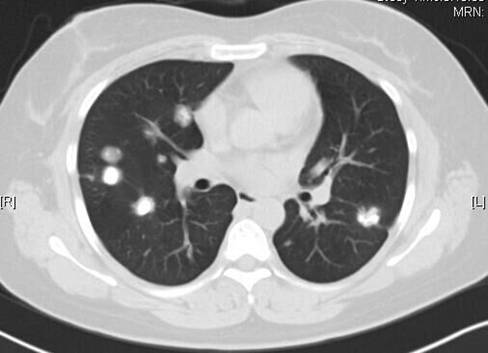
肺转移瘤的13个不典型表现(上)
2016-12-05 张嵩讲堂 医生站“张嵩讲堂”系列讲座
肺外肿瘤都是通过哪些途径转移到肺脏?每种转移瘤的影像学表现又有何特征?张嵩老师将结合6个精彩病例为您解答。








本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#不典型#
46
#转移瘤#
38
经典,得好好学习下
61
#肺转移#
25
有效控制肿瘤是非常必要的
58
值得学习
56
总结的很好
54
继续学习
67
继续关注
22