J Clin Oncol:pembrolizumab治疗复发难治的经典型霍奇金淋巴瘤有疗效
2017-04-29 任我行@血液科 肿瘤资讯
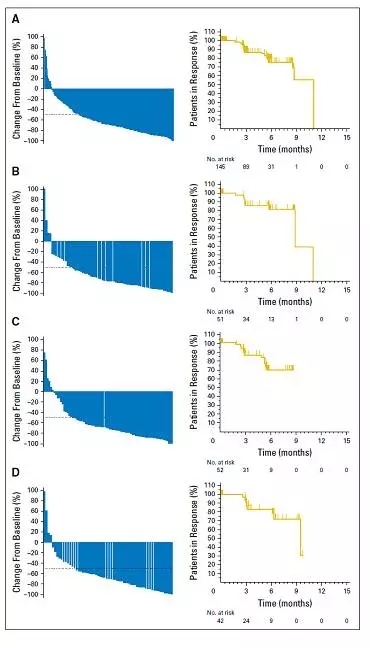
经典型霍奇金淋巴瘤(cHL)是一种治愈率很高的肿瘤,但对于放化疗难治或治疗后复发的患者,缺乏有效的治疗方案。cHL的肿瘤细胞-霍奇金Reed-Sternberg(HRS)细胞常具有染色体9p24.1的异常,这使得PD-1分子的配体PD-L1和PD-L2异常高表达,这些为在复发难治的cHL使用PD-1抑制剂提供了遗传学基础。KEYNOTE-087临床试验探索了pembrolizumab治疗复发难治的

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了.谢谢作者分享!
51
#Oncol#
33
#PE#
27
#复发难治#
31
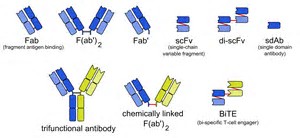
#mAb#
26
#Pembro#
30
谢谢分享,很受益
53
#Pembrolizumab#
31
为研究者们点赞
43
非常好的文章,学习了,很受益
47