Anesth Analg:术前短期血糖控制可有效减少糖尿病围手术期感染
2015-07-09 嗷大森 MedSci原创
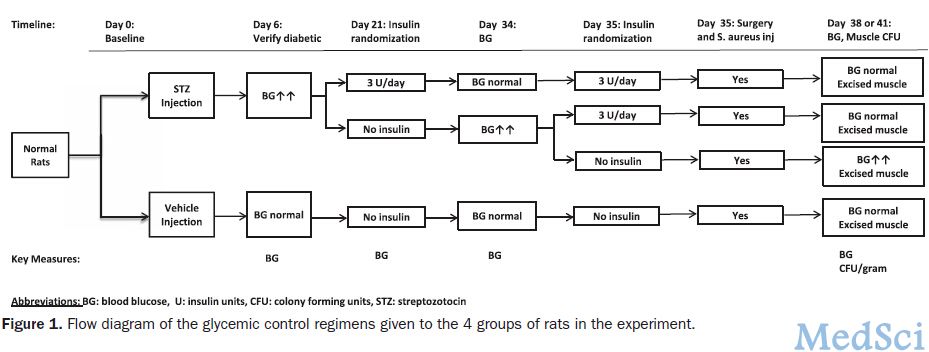
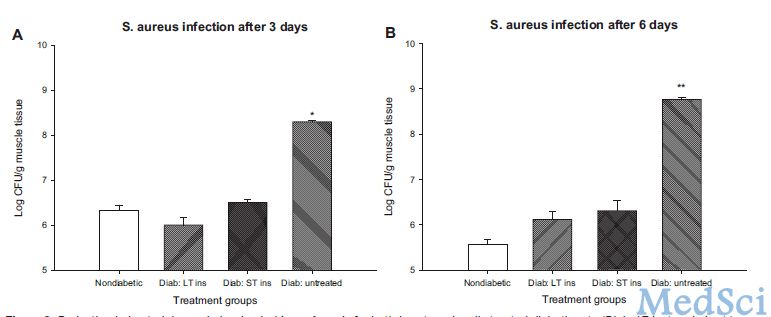
随着外科手术患者年龄范围逐渐扩大,因各种疾病需行手术治疗的糖尿病患者也日益增多。围手术期高血糖是糖尿病患者感染的独立危险因素,因为长期高血糖有利于细菌繁殖生长,加之糖尿病患者免疫功能低下,中性粒细胞功能异常、单核细胞活力下降、抗体生成减少、组织愈合能力差等,造成患有糖尿病的病人和动物更易在外科手术中出现细菌感染。 围手术期血糖的控制程度,决定患者术前等待时间长短、术后是否会出现各种并发症
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Anal#
33
#ANA#
36
#EST#
27
#手术期#
26
有道理!
156
#血糖控制#
30
看看
105