CHC 2016:阜外医院|基于互联网的高血压管理
2016-08-17 MedSci MedSci原创
2016年8月11-14日,由中华医学会与国家心血管病中心共同主办的2016年中国心脏大会在北京国家会议中心隆重召开,梅斯医学作为特约媒体参与了此次盛会。 来自北京阜外医院高血压中心主任蔡军做了题为“基于互联网的高血压管理”的精彩报告。对此,梅斯医学小编进行了整理,与大家分享。 北京阜外医院高血压中心主任 蔡军&n
2016年8月11-14日,由中华医学会与国家心血管病中心共同主办的2016年中国心脏大会在北京国家会议中心隆重召开,梅斯医学作为特约媒体参与了此次盛会。
来自北京阜外医院高血压中心主任蔡军做了题为“基于互联网的高血压管理”的精彩报告。对此,梅斯医学小编进行了整理,与大家分享。

北京阜外医院高血压中心主任 蔡军
一、我国高血压现状:
2015年6月,国家卫生计生委发布《中国居民营养与慢性病状况》,显示慢性病占中国居民死亡的86.6%,其中心脑血管疾病、癌症和慢性呼吸系统疾病占总死亡的79.4%。随之而来的是医疗费用支出的增长,2014年全国卫生总费用大35312亿元,慢病导致的医疗负担支出占总支出的70%。目前中国65周岁以上老人人数约为1.4亿人,老龄化比例逐年提高,潜在慢病人群基数势必继续扩大,社会将面临日益严重的慢病挑战。
高血压是最重要的心血管病危险因素。调查数据显示,1979~2002年间高血压发病率在逐年增加,2002年中国18岁以上成人高血压患病率为18.8%,2014年卫生部公布的高血压患病率为25.5%,全国第五次高血压调查初步数据(12个省)显示目前高血压患病率为27.9%。由此可见高血压患病率一直在增加。2010年对13省调查显示,高血压知晓率、治疗率、控制率分别为42.6%、34.1%、9.3%,高于2002年水平。
高血压是心血管疾病最重要的危险因素。70%的脑卒中、50%的心肌梗死、50%的房颤与高血压有关联。降低高血压患者的血压水平可减少40%~50%的脑卒中风险和15%~30%的心肌梗死危险。因此,控制高血压是心脑血管疾病防治的核心。
二、高血压与互联网的融合
2015年3月5日上午十二届全人大三次会议上,李克强总理在政府工作报告中首次提出“互联网+”行动计划。李克强在政府工作报告中提出,“制定“互联网+”行动计划,推动移动互联网、云计算、大数据、物联网等于现代制造业结合,促进电子商务、工业互联网和互联网金融(ITFIN)健康发展,引导互联网企业拓展国际市场。”“互联网+”的意义在于促进网络与产业的融合创新,在技术、标准和政策等多个方面实现互联网与传统行业充分对接。
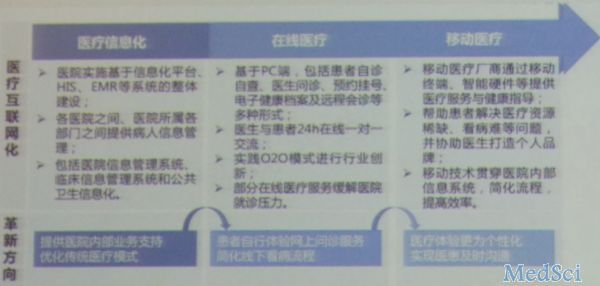
三、互联网医疗是慢病管理的发展方向
高血压领域在“移动医疗”技术方面的最新应用主要体现在传统的血压监测设备和“大数据”、“云计算”、“物联网”等移动互联网技术的创新融合上。
1 通过无线或蓝牙将移动终端APP和血压监测设备连接的这种“软硬结合”的方式,能系统的完成从“测量数据——解读数据——分享数据——靠近健康”的一个完整解决人体健康需求的闭环,对加强家庭自测血压、用药指导有很好的辅助作用。
2 医生科研通过移动医疗产品随时掌握多名患者的动态健康数据,定期检测血压波动变化,了解患者的血压是否得到满意的控制,观察药量增减的治疗效果,并作出病情预判,从而帮助医生评价治疗效果,并做出病情预判,从而帮助医生评价治疗效果,修正治疗方案。同时也能在一定程度上减轻看病难的问题,使医生患者的沟通变得更加高效。
3 移动医疗队高血压研究具有重要的学术价值,对于高血压大样本、多中心、跨地域的研究提供了极大的便利,大数据平台能帮助医生刚好地探索“疾病防治”这个大课题,助力医疗科研工作。
拓展阅读:与CHC 2016相关的拓展阅读:

蔡军,医学博士,主任医师,博士研究生导师 现任阜外医院高血压中心主任,入选国家自然科学基金优秀青年基金、教育部新世纪优秀人才、北京市高层次卫生技术人才学科带头人、北京市科技新星等。
学术兼职:心血管病国家重点实验室PI、国家心血管病中心高血压专家委员会主任委员、中华医学会心血管病学分会青年委员、中华医学会心血管病学分会高血压学组全国委员、中国老年医学学会高血压专业委员会常委兼副总干事、Cardiology Advances副主编、CNS Neuroscience & Therapeutics编委等。目前主持973课题、国家自然科学基金等课题10余项,以第一作者和通讯作者发表Circulation、Hypertension等SCI杂志20多篇。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#阜外医#
53
#高血压管理#
47
文章很好值得关注
73
开阔眼界,谢谢分享
72
好,不错,学习了。
71
值得学习
68
一个值得学习
1
#互联网#
30
#阜外医院#
39
#血压管理#
32