1例跌宕起伏的急性胸痛病例,心梗吗?
2015-03-13 中国医学论坛报 中国医学论坛报
急性胸痛是急诊内科最常见的疾病。调查发现,急性胸痛在门诊接诊的患者中占20%,在救护车接诊的患者中占69%,在急诊室接诊的患者中占45%。对于急性 胸痛首先应明确是否由潜在致死性疾病引起,如急性心肌梗死(AMI)、主动脉夹层(AD)、急性肺栓塞和张力性气胸等,需要在短时间内作出恰当诊断和处 理。若误诊或漏诊,会导致严重后果。 【病例简介】 [入院情况] 患者男性,49岁,
急性胸痛是急诊内科最常见的疾病。调查发现,急性胸痛在门诊接诊的患者中占20%,在救护车接诊的患者中占69%,在急诊室接诊的患者中占45%。对于急性 胸痛首先应明确是否由潜在致死性疾病引起,如急性心肌梗死(AMI)、主动脉夹层(AD)、急性肺栓塞和张力性气胸等,需要在短时间内作出恰当诊断和处 理。若误诊或漏诊,会导致严重后果。
【病例简介】
[入院情况]
患者男性,49岁,因“突发胸痛2小时”来诊。患者来诊前2小时于散步中突发心前区疼痛,压迫样、剧烈难以忍受伴大汗,呈阵发性,最长持续30分钟,发作间歇胸痛可完全缓解。
查体示血压85/55mmHg(双侧肱动脉),心率50次/分,律齐,未及心脏杂音,四肢肢端暖。神志清,双肺呼吸音清,未及干湿音。否认高血压、糖尿病史。
心电图示Ⅲ、aVF导联ST段弓背抬高0.05mv,V4~V6导联ST段下斜形压低0.1~0.2mv,冠状窦心律(图1)。
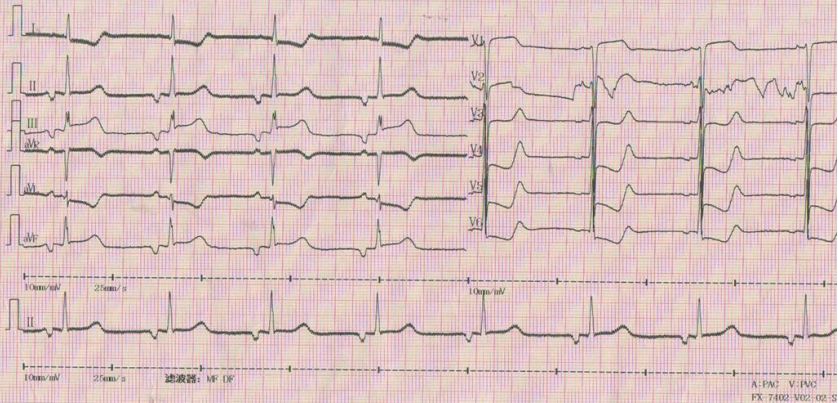
图1 入院心电图
[急诊处理]
给 予生理盐水快速补液、多巴胺10μg/kg·min持续滴注、吗啡3mg iv.对症止痛,并行血常规、肝肾功能、肌钙蛋白I(TNI)和D-二聚体(D-Dimer)检测,等待结果。经治疗后胸痛缓解。来诊后25分钟再次出现 剧烈胸痛伴大汗,复查心电图示Ⅱ、Ⅲ、aVF导联ST段进一步抬高,并出现Ⅲ度房室传导阻滞(AVB),心率降至40次/分(图2)。诊断为急性下壁心肌 梗死、Ⅲ度房室传导阻滞(AVB),加用异丙肾上腺素持续滴注。
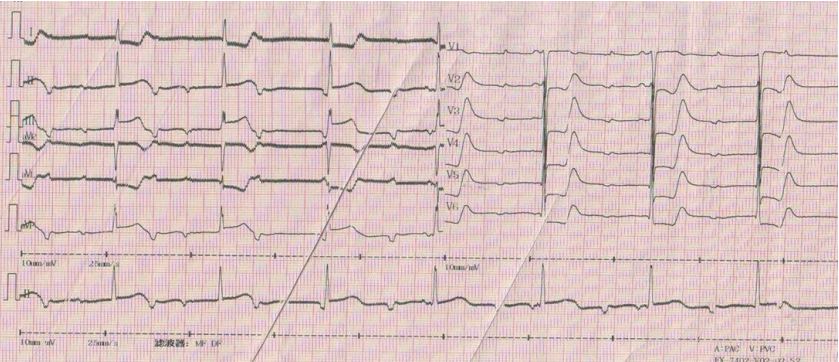
图2 来诊后25分钟心电图
诊 断明确后,决定行直接经皮冠脉介入治疗(PCI)及急诊临时起搏器置入术。术前予阿司匹林300mg、氯吡格雷300mg嚼服,普通肝素5000u静推。 穿刺股动、静脉,测右股动脉压90mmHg,心率30次/分,Ⅲ度AVB(给予多巴胺10μg/kg·min、异丙肾上腺素持续滴注),经股静脉置入临时 起搏器。冠状动脉造影提示右冠脉(RCA)开口90%狭窄(未见明显血栓)、左冠脉(LAD)远端90%狭窄、左回旋支(LCX)中段70%狭窄。决定于 RCA开口行经皮冠脉腔内成形术(PTCA)+支架置入术。RCA开口以Sprinter2.5×15球囊14atm扩张(Door-Balloon时间 40分钟),乐普4.0×18mm支架于RCA开口14atm扩张,支架内予Dura Star4.0×15mm后扩张球囊20atm扩张,RCA开口无残余狭窄,远端血流TIMIⅢ级(图3)。于RCA开口行球囊扩张后,血压上升至 105mmHg,心率上升至60次/分。患者术中出现室性心动过速,心率140次/分,予胺碘酮150mg静推后转律,术后胸痛完全缓解,收入监护室。

图3 术中冠脉造影
[病情突变及转归]
监护室心电图示Ⅱ、Ⅲ、avF导联ST段较前明显恢复,术后1小时停用多巴胺,5小时转为窦性心律并持续存在(图4)。至此,患者临床情况似乎稳定,继续常规抗栓治疗。
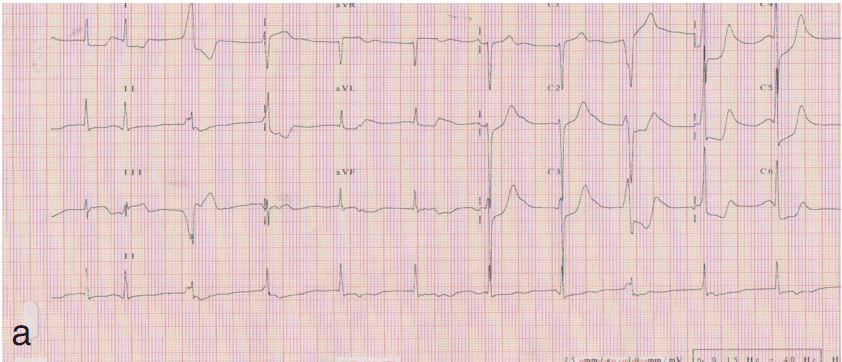
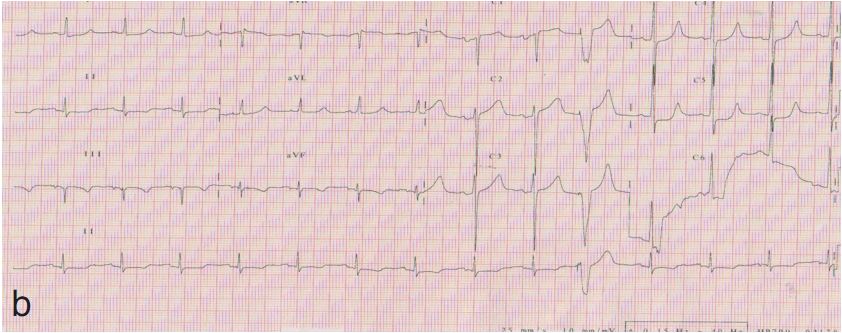
图4 术后复查心电图
来诊后2小时 各 项实验室检查回报,结果示D-Dimer5628ng/ml。此时医生意识到患者D-Dimer异常显著升高,与AMI诊断不匹配,或许有其他诊断可能。 急行床旁超声心动检查,见升主动脉内径47mm,主动脉根部及升主动脉、腹主动脉内径明显增宽,主动脉根部紧邻无冠瓣瓣根处及右冠瓣瓣上见游离剥脱内膜片 回声,延伸至腹主动脉,主动脉根部真腔内径31mm,假腔内径15mm,主动脉瓣中重度反流。急行主动脉血管造影(CTA),示升主动脉夹层,累及主动脉 弓、降主动脉、脾动脉、左肾动脉(图5)。监测心肌标志物,不符合AMI酶学变化(表1)。
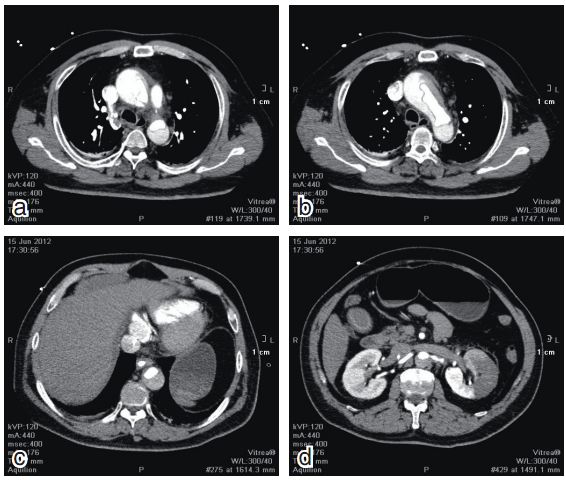
图5 CTA示升主动脉夹层,累及主动脉弓、降主动脉、脾动脉、左肾动脉
表1 心肌标志物变化

距发病5小时 最终诊断为主动脉夹层(AD,A型)、主动脉瓣重度关闭不全,急性下壁心肌梗死、Ⅲ度AVB,急性肾损伤,急性肝损伤。其中急性下壁心肌梗死、急性肾损伤、急性肝损伤均由AD累及所致。明确诊断后急请心脏外科会诊,建议先行内科保守治疗,控制心率及血压。
距发病10余小时 出现急性肝损害、急性肾损害、急性骨骼肌坏死和代谢性酸中毒,联合应用连续性肾脏替代治疗(CRRT,无肝素)。
距发病42小时 患者突发心跳、呼吸停止,抢救无效死亡。死亡原因为AD破裂。
【讨论】
AMI和AD,一对难兄弟
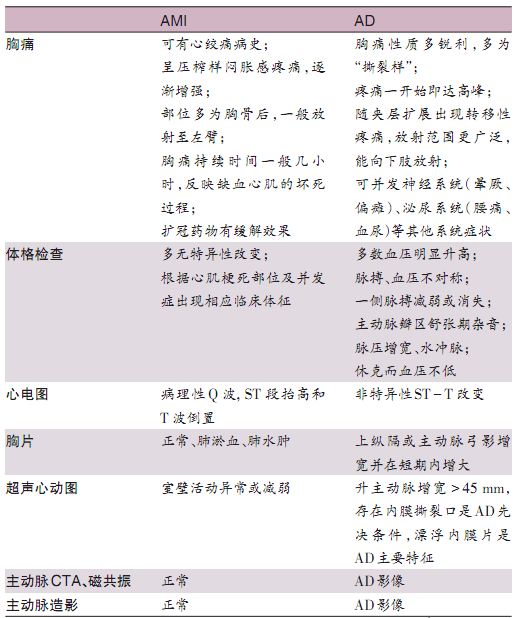
AMI 和AD临床均可表现为急性胸痛,若出现持续剧烈胸痛伴有以下情况时应怀疑存在AD:①剧烈疼痛,向背部、下腹部放射明显,吗啡镇痛效果欠佳;②闻及心脏杂 音,特别是主动脉瓣区新出现的杂音;③突发肾绞痛或血尿,伴肾功能不全;④四肢脉搏不对称,特别是双上肢血压不对称、血压与休克表现不相符;⑤心电图及心 肌坏死标志物不符合AMI演变过程。总结为3个不对称,胸痛与心电图表现不对称、症状与体征不对称、血压与休克表现不对称。典型AMI和AD患者并不难诊 断(表2),但对于复杂、合并病例,快速准确地进行临床鉴别较困难,存在以下几个问题:①是AD还是AMI?②若合并,是夹层累及冠脉导致AMI,或是 AD应激诱发AMI,或是两者平行存在?③若患者已有冠心病或心肌梗死病史,再发严重胸痛,能不能克服惯性思维,想到AD可能?
表2 AMI和AD鉴别诊断要点一览
反思及体会
该 患者在初始阶段主要表现为急性下壁心肌梗死,经直接PCI治疗后胸痛暂时缓解、生命体征暂时稳定,但随着诊断、治疗的推进不断有疑问产生,胸痛剧烈程度为 何与心电图变化不匹配?右冠脉造影显示的血栓负荷情况为何与心肌梗死疾病不匹配?D-Dimer异常显著升高为何与AMI诊断不匹配?以上临床情况与客观 检查的不匹配,即使在胸痛和生命体征好转后仍不能得到解释。随着最终诊断的水落石出,以上疑问也迎刃而解,原来急性下壁心肌梗死、急性肾损伤、急性肝损伤 的根本原因都是AD。
从 该病例中笔者得到以下体会。AD合并AMI时鉴别困难,仍可从以下6个方面进行鉴别:①心电图非典型心肌梗死表现,且与胸痛程度不匹配;②AMI合并四肢 动脉血压不对称、主动脉瓣关闭不全、与心肌梗死不相关的意识障碍、肾功能不全应警惕AD;③AMI合并D-Dimer异常严重升高应警惕AD;④AMI 时,X线胸片提示纵隔增宽应警惕AD;⑤AMI时,超声心动图示升主动脉内径>45mm应警惕AD;⑥PCI术中常规透视纵隔,若发现纵隔增宽,行升主动 脉造影明确AD。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学到了
73
彩超真的非常重要!!!之前收一个急性下壁AMI+三度AVB的,导管室台都开好了,临时加了个彩超发现主动脉根部宽,于是做的CTA,右窦被撕了,一直到肾动脉。。。
64
谢谢病例,学习一下
4
谢谢,学习病历,就是学习
58
好病历,确实可以先做个主动脉根部的造影
100
很不错!
45
好病例
89