J Neurosci:新标志物有助诊断阿尔茨海默病
2012-06-18 陈蓉 生物谷
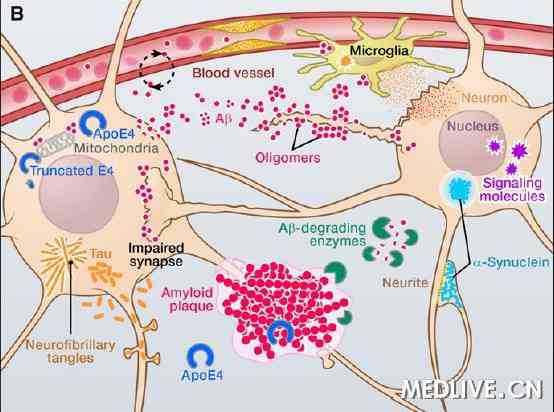
近日,波士顿大学医学院(BUSM)研究人员确定阿尔茨海默病患者大脑中一种积聚的蛋白质组。这些调查结果发表在Journal of Neuroscience杂志上,该研究可能有助开辟新的方法来诊断治疗阿尔茨海默病患者。[J Neurosci 2012 Jun 13;32(24):8270-83] &n
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#标志物#
44
#阿尔茨海#
41
#阿尔茨#
50
#ROS#
39
#阿尔茨海默#
42